
Miriam Reichel (MR) interviews Dr. med. Ute Krüger (UK)
MR: I am very pleased to have a conversation today with Dr. Ute Krüger. You are a pathology specialist and senior physician at a municipal hospital in Sweden.
Many cancer patients are unsure about the effects of the Corona vaccine on their cancer. So far, most oncologists recommend the vaccinations, even though there are no studies in cancer patients yet. In the next few years, it will be very interesting to see if the vaccination has any negative effects on tumor incidence in the population.
My name is Miriam Reichel. I had terminal cancer in 2004 and have been completely healthy since 2005. I have written several books on the subject of cancer and healing. Therefore, I am particularly interested in the influence of the environment and medicine on cancer.
1) Would you like to say something else about yourself, Ute?
UK: I am very happy to be able to talk to you today, dear Miriam. I have been very touched by your life story so far, especially the healing of your terminal cancer. This showed me once again that there is a lot that we conventional doctors don’t know, and that we have to be much more open, as there is still an incredible amount to be researched.
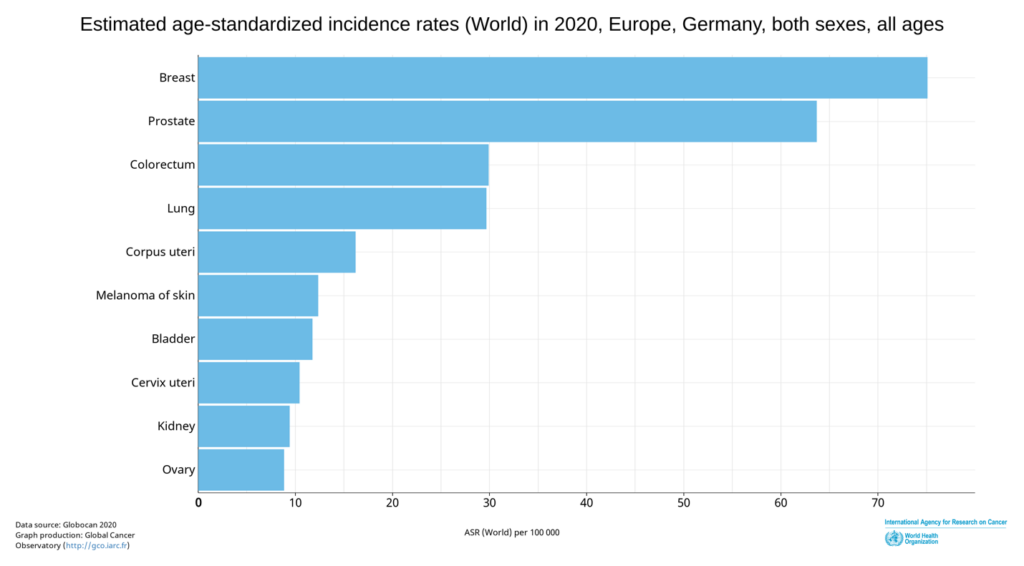
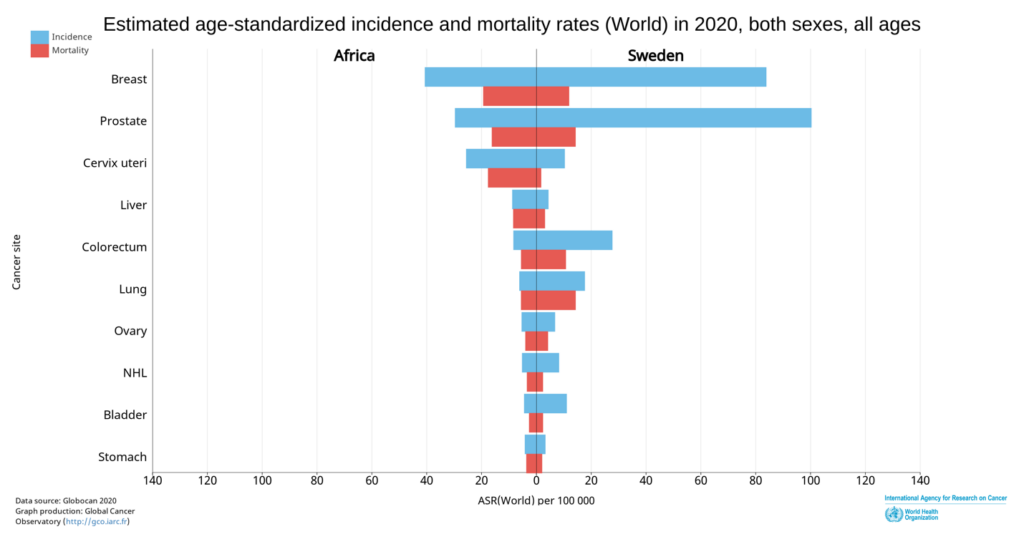
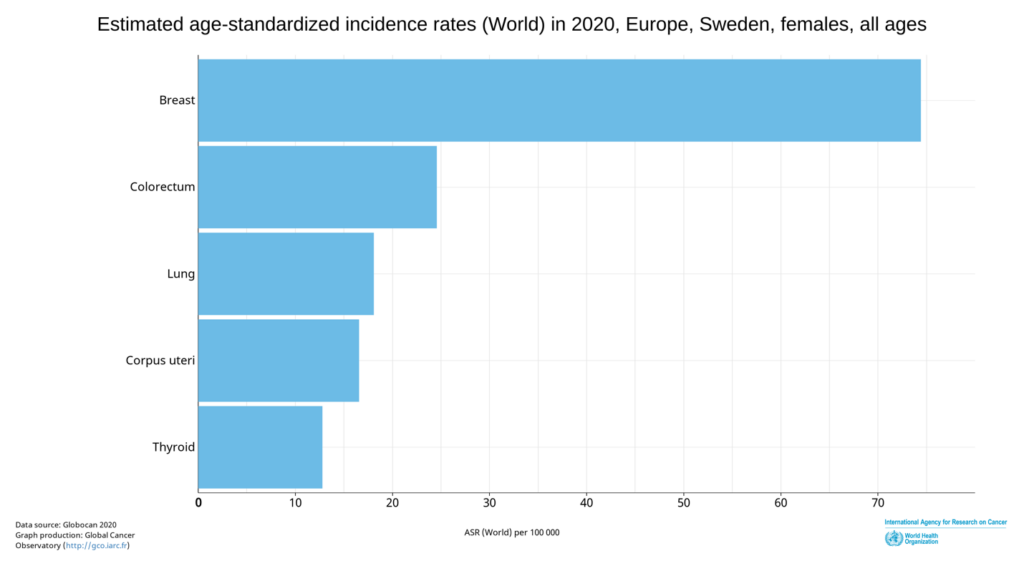
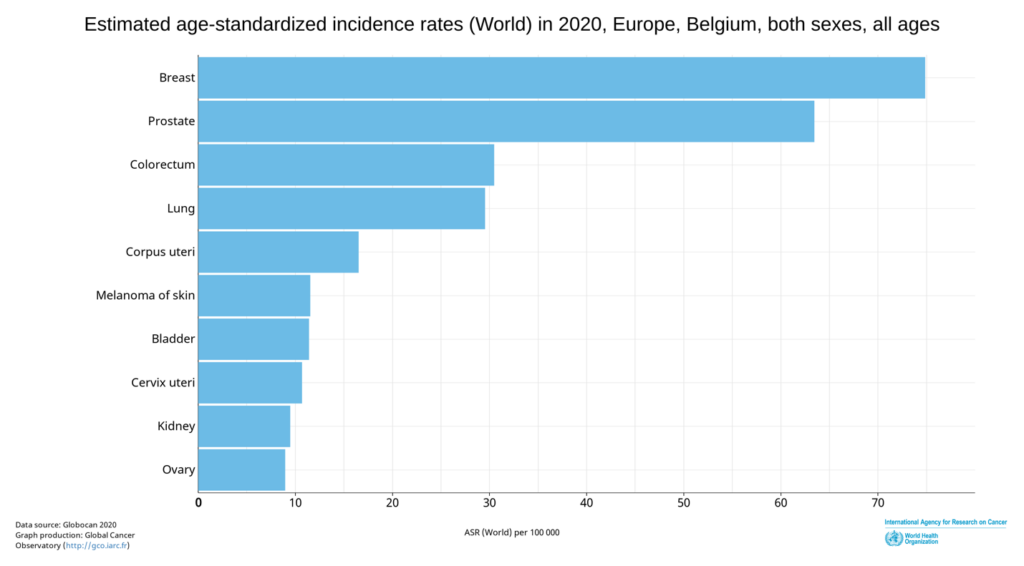
2) MR: The cancer rate in Europe is continuously increasing. In 2020, breast cancer was leading. Germany has 70.4 cases per 100,000. In Sweden, the rate is even higher at 73.4. Belgium has the most breast cancer cases in Europe. Now it is often claimed that the new Corona vaccine could increase the cancer rate even more.
You have been working as a pathologist primarily in breast cancer for 18 years. Have there been any changes recently?
UK: For a better understanding, I would first like to explain the work of a pathologist. The widespread opinion, unfortunately also among some physicians, is that pathologists deal exclusively with the autopsy of deceased persons.
However, the main occupation of a pathologist is to examine tissue samples from living patients. The result of this examination then lays the foundation for the subsequent therapy of the patients. Without pathologists, there would be no tumor treatment in the traditional medical sense.

And now to the real question, have I noticed any changes lately?
In the last few months I feel that the tumors in the breast are bigger. Here in Sweden there is a very well-functioning mammography screening program.
Women aged 40-74 have the opportunity for regular radiological check-ups to detect tumors in the breast at an early stage. So, it has been rare to see tumors larger than 3 cm in my examination material. Now I see tumors that are not infrequently larger than 4 cm. Tumors of 5 cm, 6 cm, 10 cm and in the last week even 16 cm, i.e. occupying the whole breast, used to be rarities but are now found in my examination material.
In addition, I feel that the patients are younger. I have reviewed 1500 breast cancer cases in the last six years in my population-based research material, so I have an idea of how old patients usually are when they develop breast cancer, not only through daily routine preparations but also through research. Recently, it is not uncommon for me to see breast cancer cases from patients who were born in the 70s and 80s and occasionally in the 90s, which means they are 35 to 50 year old patients.
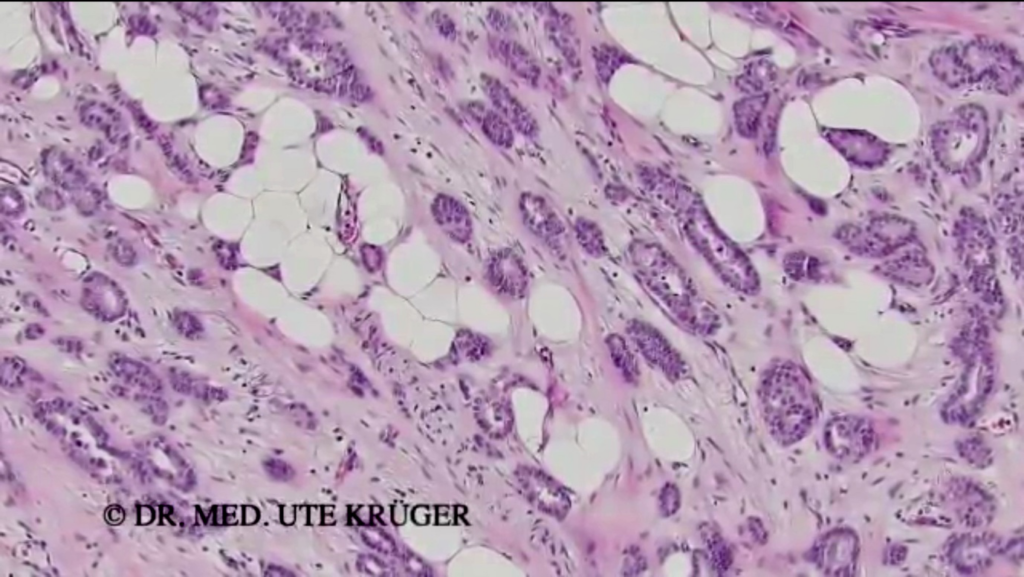
In addition, I have the impression that the tumors are growing more aggressively, i.e. are more poorly differentiated. I would like to illustrate this with two images. Here you can see a sectional preparation in 150x magnification, i.e. an approximately 4 micrometer thin section of the tumor tissue, which has been stained to make it easier to see. Here you can see glandular-like associations that often occur in better differentiated breast cancer cases.
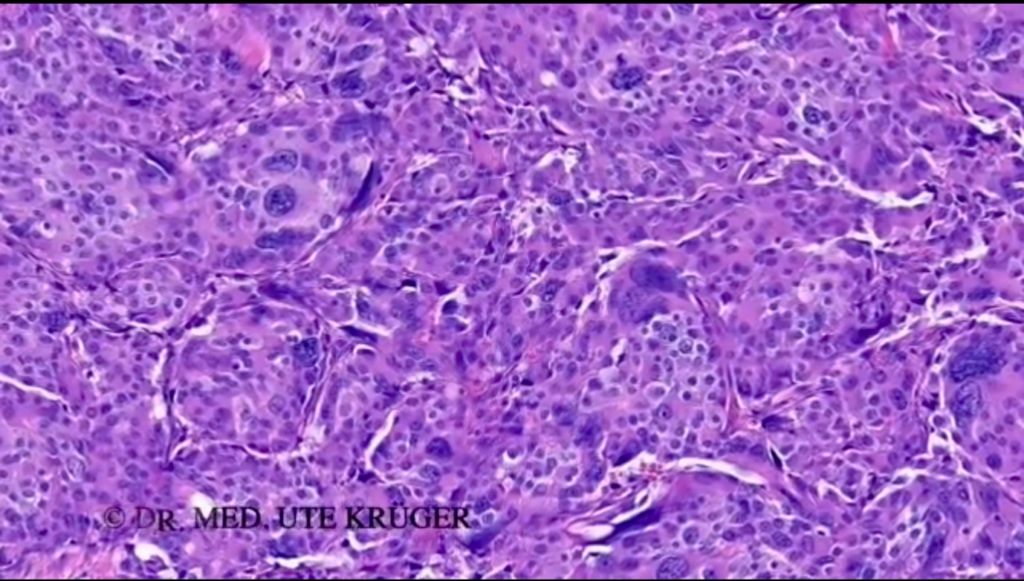
In the next image, one sees an aggressively growing tumor, i.e., no glandular-like dressings as in the previous image, but often solid, i.e., compact tumor growth. The cells show larger nuclei.
MR: Thank you, that’s very interesting!
There is often mention of the Ki-67 factor – a protein that is used to mark dividing cells – and that there is now a higher factor than usual, so faster cell growth.
What makes the fast cell growth so negative and what could you observe in this area?
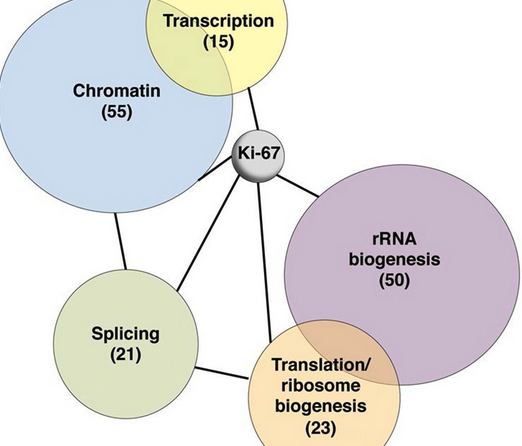
UK: This fits together with what was said last time. The tumors seem to grow more aggressively, the cells divide more frequently. I see in the sectional preparation many mitoses, i.e. nuclear division figures, which I have marked with arrows. Ki-67 is an antibody that stains the cells that are in the active phase of the cell cycle, for example, also in the mitotic phase. So if there are many cells in division, many cells will be labeled with Ki-67.

At this point, I can perhaps address the problems of an aggressively growing tumor. Slower growing small tumors are often removed surgically, i.e. with one operation. If the tumors are larger, however, lymph node metastases may already be found, i.e. tumor spread far from the actual site of origin in the breast. In this case, tumor treatment is often started with chemotherapy, a so-called neoadjuvant treatment. Only after months of chemotherapy is surgery then performed. The operation is usually followed by radiotherapy of the breast and/or armpit.
4) MR: There are low and high Ki-67 values. Which values could you observe?
UK: In this regard, it is important to know that about 2/3 of malignant breast tumors are less proliferative, i.e. have a lower Ki-67 value, and about 1/3 of malignant breast tumors are highly proliferative, i.e. have a higher Ki-67 value. For example, a very slow growing tumor shows a Ki-67 value of 10%. This means that 10% of the cells in the tumor are undergoing cell division. Here in the picture, the cell nuclei are colored brown. All other cell nuclei, faintly stained blue, are negative for Ki-67, i.e. not in cell division.
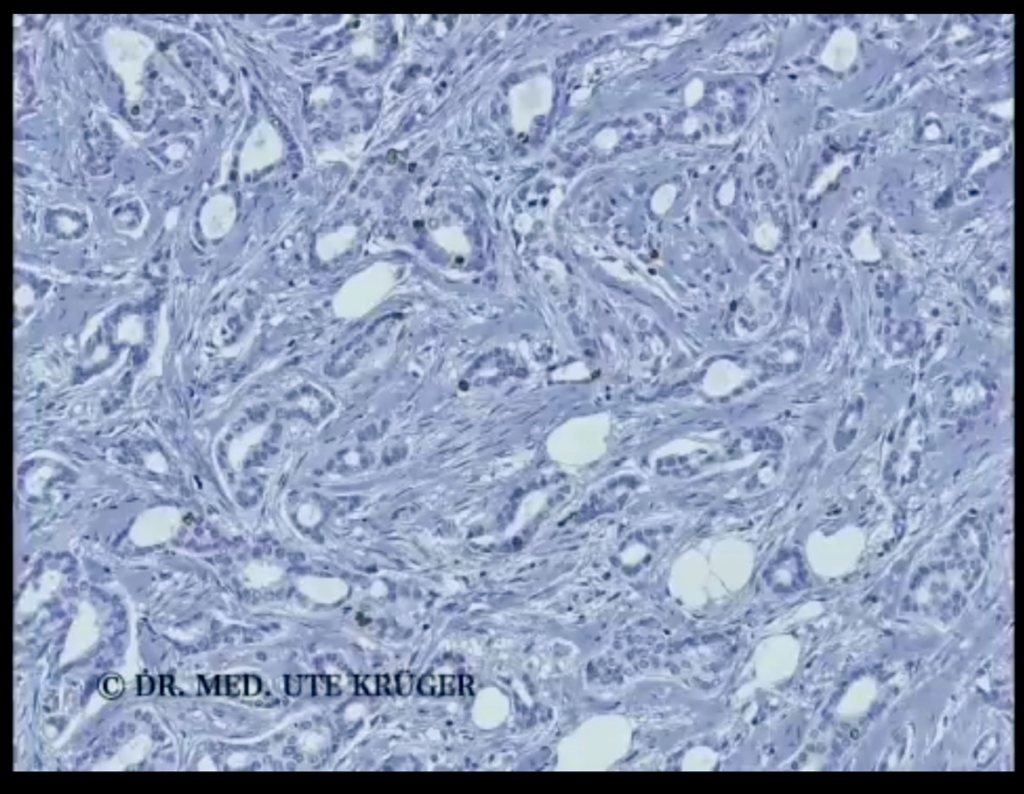
Faster growing tumors have a much higher Ki-67 value, for example 35 %. Here many more cells are in division. I have the impression that I now more frequently see tumors in the examination material that have Ki-67 values of 50 % as here in the picture, 75 % or more. This means that half, 2/3 or even more of the tumor cells are in cell division, which means that the tumors are growing extremely fast.
5) MR: Inflammatory processes are increasingly perceived as side effects after vaccination. Primarily, we are aware of myocarditis, and inflammatory autoimmune diseases, such as vasculitis.
Cancers usually have their origin in inflammatory processes.Could these processes cause more cancer cases?
UK: This cannot be ruled out.
For example, there is a higher risk of breast cancer in overweight women. One theory is that the altered adipose tissue function and the death of fat cells leads to a low level of chronic inflammation, which in turn promotes the development of tumors.
It will therefore become clear in the course of the next few years what influence these autoimmune diseases, i.e. inflammatory changes, which appear to have arisen after vaccination, have on the development of tumors.
6) MR: It is often claimed that the immune system overreacts due to vaccination and lymphocyte infiltrates are also increased.Can this process have an effect on a tumor?
UK: This is closely related to the previous question. Lymphocytes belong to the group of white blood cells that perform specific tasks in the defense against pathogens. In some malignant breast tumors, so-called tumor-infiltrating lymphocytes are found, i.e. inflammatory cells in the tumor. This is a topic I deal with in my research. Here I reviewed breast carcinomas diagnosed in the years 1996-2014. It is important to distinguish whether it is tumor growth stimulating or tumor growth inhibiting inflammatory cells in the tumor. What influence the apparently vaccine-triggered exuberant immune response has on tumor growth will be shown by research in the coming years.
7) MR: The prestigious New England Journal of Medicine reported on trials of RNA vaccines against SARS and MERS, which had to be discontinued because animal studies showed that there was a severe autoimmune reaction with inflammation of the lung tissue1. This was attributed to an overreaction of type 2 T helper cells, which regulate the strength of an immune response. Normally, T cells are particularly effective against both infected and abnormal cells.
Can this lead to a situation where our immune system no longer acts against cancer cells?
UK: The immune system, our built-in defense system in the body, is very complex. I would like to try to explain it in a simplified way and then answer your question.
There is the non-specific, innate defense and the specific, acquired defense. The optimal interaction of these two defense mechanisms allows us to stay healthy. It protects us from pathogens, such as bacteria, viruses and parasites, but also from the development of cancer, which is caused by a defective change in our own body cells.
The nonspecific immune response first responds to the penetration of a pathogen by activating granulocytes, macrophages, and dendritic cells. All of these are phagocytes. Both the dendritic cells and the macrophages break down the pathogen inside them and present fragments of it on their cell surface and circulate around the body. This is when the specific immune response comes into play.
The specific defense cells, the lymphocytes as specialists of the human defenses, are mobilized. Through the interaction of the phagocytes with the T cells, the killer cells (or cytotoxic T cells, as they are actually called) are activated via type 1 helper cells. These killer cells eliminate the cells infected with the pathogen or the defectively formed pathological cells in our body.
The most important function of the type 2 helper cells you mentioned is the activation of the B cells, i.e. the antibody-producing cells.
If overactivation occurs, an autoimmune disease develops, as described in the mentioned article in animal experiments.
If there are too few type 2 helper cells, one sees the picture of AIDS, the body becomes susceptible to numerous diseases.
Now to your actual question: If, for example, the function of the killer cells is impaired by the injection of these substances, cancer could develop in this way.
However, the immune system is much more complex than I have described and it is still unclear which mechanisms might be at work here.
8) MR: Are there also observations on the change of tumor growth in existing tumor diseases?
UK: I have been able to observe individual cases where vaccination against Covid-19 seems to have led to a change in the aggressiveness of the tumor. One breast cancer patient had known metastases, i.e. a spread of her breast cancer in the body, for many years. Shortly after vaccination against Covid-19, the tumor growth of the metastases exploded in the liver, but not in the skeleton or other affected internal organs. In the sectional preparation, I could see the original relatively slow-growing tumor with a relatively low Ki-67 value, but in addition, a very aggressive tumor component with a very high Ki-67 value.
Again, we will have to wait and collect data to draw conclusions.
9) MR: I have often read the term ‘insertional mutagenesis’ in this context. What is feared in particular is the activation of cellular proto-oncogenes2. The Corona vaccines could cause activation of oncogenes or deactivation of anticarcinogenic DNA sequences, thereby increasing tumor risk3.
Can you explain these terms to me? Could this increase the risk of cancer?
UK: I am not a geneticist, but insertion is first of all the insertion of a DNA segment into the DNA sequence (sequence is the sequence of the basic chemical building blocks of DNA). The DNA contains the genes of a cell.
In insertional mutagenesis, a mutation, i.e. a change in the DNA, is induced by inserting one or more base pairs. This is used in research or can also be induced naturally, such as by viruses.
Proto-oncogenes are normal genes of the cell that control and moderate cell growth and proliferation. Mutation, i.e. alteration of the genetic material, of a proto-oncogene can transform it into an oncogene. Oncogenes ensure that gene regulation no longer functions and cancer develops.
In insertional mutagenesis, a mutation, i.e. a change in the DNA, is induced by inserting one or more base pairs. This is used in research or can also be induced naturally, such as by viruses.
Proto-oncogenes are normal genes of the cell that control and moderate cell growth and proliferation. Mutation, i.e. alteration of the genetic material of a proto-oncogene can transform it into an oncogene. Oncogenes ensure that gene regulation no longer functions and cancer develops.
In this context, on the genetic level, it is important to mention that Swedish researchers were able to determine in vitro, i.e. in experiments in an artificial environment (PMCID: PMC8538446), that the SARS-CoV-2 spike protein impairs the DNA repair mechanism. Should this also be proven in vivo, i.e. in the living organism, this would mean that the DNA repair mechanism would be damaged by the spike proteins, possibly resulting in cancer. That would be terrible!
MR: Is there anything else you would like to add?
UK: Yes, that we humans treat each other with respect again. That we reduce aggression by listening to each other again. And thus love comes into our lives again.
_________________________________________________________________________________________
1 Developing Covid-19 Vaccines at Pandemic Speed
2 The past, current and future trends in DNA vaccine immunisations – ScienceDirect
3 The past, current and future trends in DNA vaccine immunisations – ScienceDirect